Let's Stop Gaslighting Gluten as a Second Class Food Allergen & Celiac as Not a Food Allergy!
- Jon Bari

- Mar 11, 2023
- 29 min read
Updated: Feb 20, 2025

"What’s in a name?
That which we call a rose by any other name would smell just as sweet."
-- William Shakespeare
Shakespeare used this famous "What’s in a name" line in Romeo and Juliet to convey that the naming of things is irrelevant. However, I disagree with that assertion when it comes to the terms "food allergy" and moreover "food allergen." Is Celiac Disease a food allergy, auto-immune disease and/or digestive disease? Spoiler alert - it's all three. However, with respect to the consumer protection needs of the Celiac community with food labeling, Celiac Disease is a food allergy and Gluten is a food allergen. Period. Full Stop.
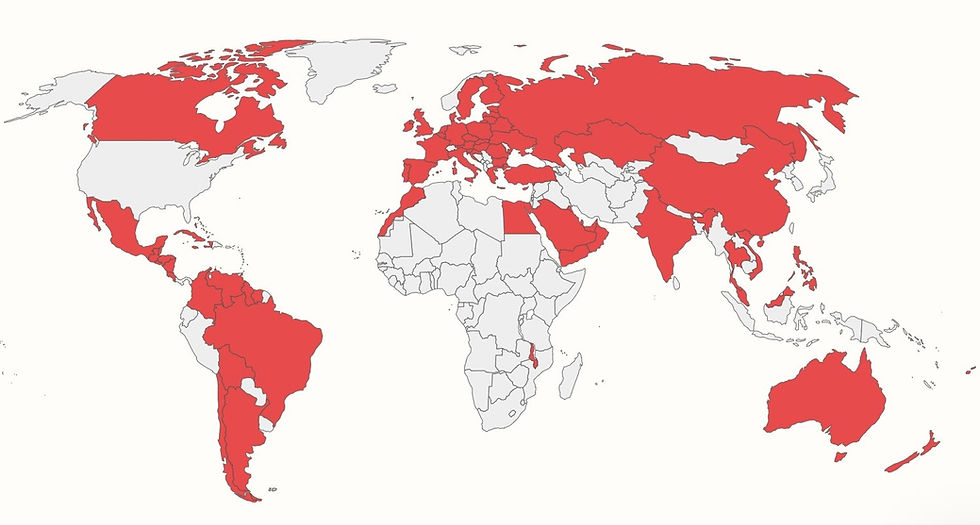
Biomedically, conversationally and legally, it's time for regulators, scientists, doctors, consumers and the food allergy community (even including the Celiac community) to stop gaslighting Gluten as a second class food allergen and Celiac as not a food allergy when it comes to consumer protection with labeling Gluten as a Major Food Allergen in the US. Our policy objective is in alignment with the conclusions of the 2021 Expert Consultation from the Food and Agriculture Organization of the United Nations and World Health Organization (chaired by the FDA's Dr. Lauren Jackson) and how 85 other countries label Gluten as a Major Food Allergen to provide consumer protection for Celiacs.
What is Food Allergy? The Similarities and Differences Between Non-IgE-Mediated Mechanisms with Celiac Disease & Typical IgE-Mediated Mechanisms
According to the National Academies of Sciences, Engineering, and Medicine, Committee on Food Allergies, "Food allergy has two key classifications: immunoglobulin E (IgE)-mediated or non-IgE-mediated."

There are several very important near-peer similarities between a Celiac food allergy with Non-IgE-Mediated Mechanisms (Gluten) and typical IgE-Mediated Mechanisms (Milk, Eggs, Fin Fish, Crustacean Shellfish, Tree Nuts, Peanuts, Wheat, Soybeans & Sesame): potentially life-threatening, the only treatment is to strictly avoid the food allergen(s), and consumers’ reliance on food labels to know what is safe to eat. Importantly, unlike food allergies with IgE-Mediated mechanisms, there is no rescue medicine (i.e., adrenaline or antihistamine) to treat accidental ingestion of Gluten and the start of the auto-immune cascade in food allergy with Non-IgE-Mediated mechanisms such as Celiac Disease. Additionally, those with a Non-IgE-Mediated food allergy to Gluten cannot outgrow their food allergy – Celiac is lifelong (until such time as a cure may be developed).[1]
Celiac Sits at the Intersection of Food Allergies, Auto-Immune Diseases & Digestive Diseases
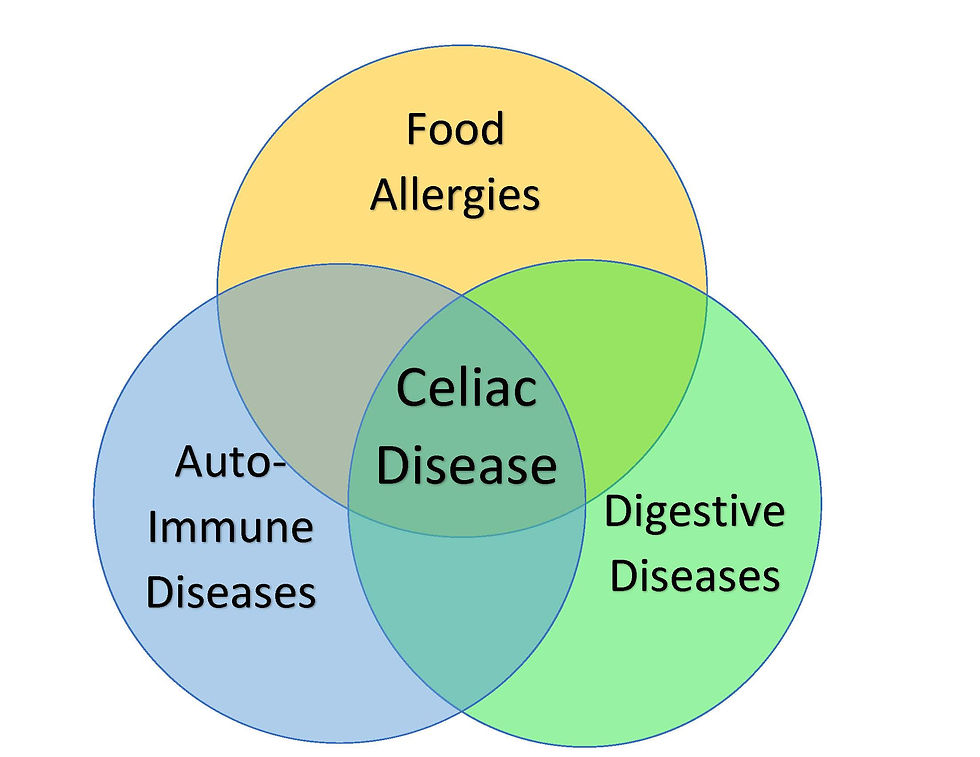
While there are many similarities between food allergies with IgE-Mediated Mechanisms and Non-IgE-Mediated Mechanisms, including needing the same consumer protections with food labeling, it is also instructive to understand how Celiac Disease is uniquely complex since it sits at the intersection of food allergies, auto-immune diseases and digestive diseases. The Venn diagram shows how Celiac can often be misunderstood. The complexity of this amalgam has seemingly made it more challenging for public servants, scientists, doctors and the Celiac community to address and protect the Celiac community’s food safety needs. A review of various descriptions of Celiac Disease and programs related thereto from Federal government agencies suggests that this complexity has also enabled the othering by various government officials of a food allergy with Non-IgE-Mediated mechanism for Celiac to be considered something other than/less serious than a food allergy and Gluten something other than/less serious than a food allergen.
Definition of Food Allergy: Celiac is a Food Allergy and Gluten is Food Allergen that Triggers Celiac
According to the FDA, "A food allergy is caused by a naturally-occurring protein in a food or a food ingredient, which is referred to as an 'allergen.'" In answering the question, "What is Gluten?", the NIH's National Library of Medicine stated that Gluten is a food protein, and that Gluten containing grains include Wheat, Barley, Rye and Oats. According to the NIAID's (National Institute of Allergy and Infectious Disease’s) Sponsored Expert Panel found, "A food allergy is defined as an adverse health effect arising from a specific immune response that occurs reproducibly on exposure to a given food."
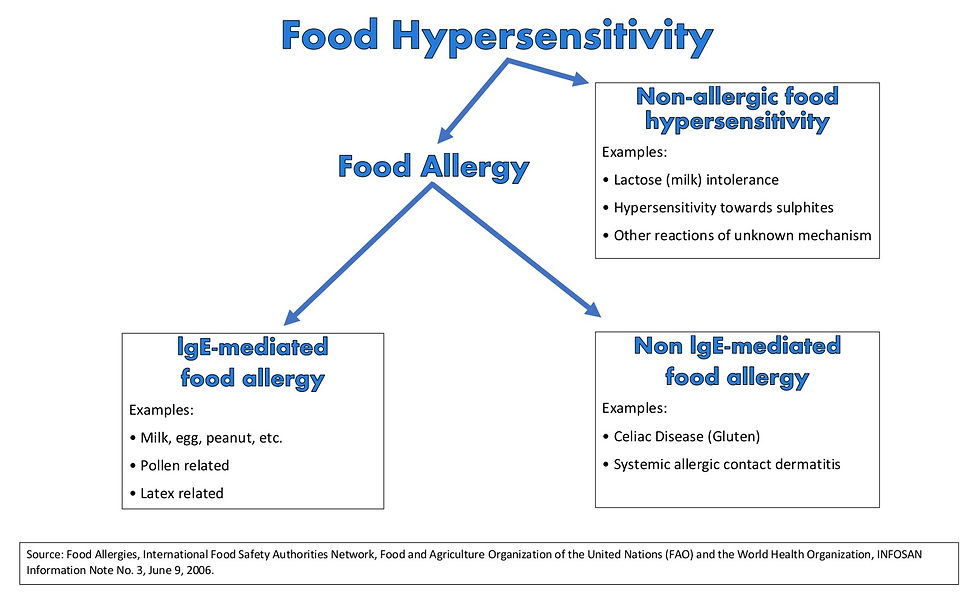
According to the FDA, "Food allergy is a form of food hypersensitivity. Adverse reactions to food due to food hypersensitivity can be broadly grouped into reactions that are mediated by either immune mechanisms (food allergic reactions) or non-immune mechanisms (primarily food intolerances). Adverse reactions that are immune-mediated can be caused by:
IgE-mediated mechanisms (e.g., IgE-mediated anaphylactic reaction to peanuts);
Non-IgE-mediated mechanisms (e.g., adverse reaction to gluten in the case of celiac disease);
Mixed immune mechanisms (e.g., eosinophilic gastroenteropathies); or
Cell-mediated mechanisms (e.g., contact dermatitis)."
Food Hypersensitivities Range from Non-Allergic Food Intolerances to Potentially Life-Threatening Food Allergies
Food hypersensitivities range from intolerances to allergies.
Dietary Spectrum: What is Food Preference, Food Intolerance and Food Allergy?
While food allergies are much more serious than food intolerances, a Gluten food allergy too often incorrectly gets conflated with food intolerances or voluntary food preferences (i.e., Gluten Free lifestyle, vegan, vegetarian). Celiacs do not have the luxury of a food preference for Gluten Free, and Celiacs do not have a food intolerance or sensitivity to Gluten! The only available treatment for Celiacs is a strict lifetime Gluten Free diet. Celiacs have a food allergy to Gluten since the ingestion of Gluten causes an immunological response.
"Celiac Disease food allergy must be treated as seriously as IgE-Mediated food allergies. Celiac must also not be conflated with Gluten Intolerance (Non-Celiac Gluten Sensitivity) or a voluntarily chosen Gluten Free lifestyle."
In medicine, mechanism in action is used to describe how, for example a drug or food allergen in this case produces an effect in the body. While Celiacs may endure digestive symptoms with Gluten ingestion, the digestive system is a downstream mechanism whereby the ingestion of Gluten causes an immunological response (non-IgE-Mediated) that can then impact the digestive system with short-term GI issues (i.e., diarrhea, vomiting, abdominal pain, etc.) and long-term health effects (i.e., anemia, cancer, failure to thrive, heart disease, immunological scarring, infertility, intestinal damage, malabsorption, malnutrition, migraines, etc.).
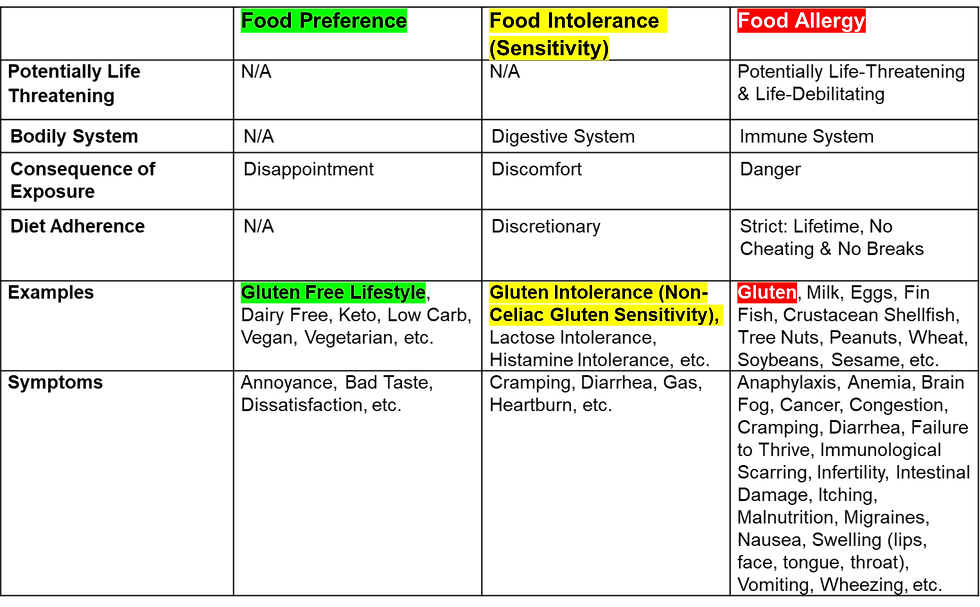
According to the American Academy of Allergy, Asthma & Immunology (AAAAI), "Eating a food you are intolerant to can leave you feeling miserable. However, if you have a true food allergy, your body's reaction to this food could be life-threatening." In discussing the digestive system versus the immune system, the AAAAI stated, "A food intolerance response takes place in the digestive system. It occurs when you are unable to properly breakdown the food. This could be due to enzyme deficiencies, sensitivity to food additives or reactions to naturally occurring chemicals in foods. Often, people can eat small amounts of the food without causing problems. A food allergic reaction involves the immune system. Your immune system controls how your body defends itself."
It is instructive to understand the consequence of exposure (ingestion) as illustrated in the chart above. For someone with a food preference, the consequence of exposure can be disappointment, whereas for someone with a food intolerance, the consequence of exposure can be discomfort. This is in stark contrast to someone with a food allergy whereby their consequence of exposure can be danger (i.e., life-threatening).
Our Lived Experience - Jax Has a Severe Food Allergy to Gluten
When Jax was diagnosed with Celiac in 2018, we were informed that the only available treatment was a strict Gluten Free diet for life, and that if he ate Gluten, he would get very sick and continue to damage his small intestine. We intuitively thought of Celiac in the context of a food allergy as many consumers and lay people do. As the Boston Globe reported in 2015, Harvard's Dr. Alessio "Fasano now gives his celiac patients permission to use the word allergy to describe their disease, since that will probably be taken more seriously." I loved that when I first read it years ago, but fast forward to 2023, and I think that we need to do much more than give permission. In terms of consumer protection with food labeling, the Celiac community would benefit greatly if the FDA, doctors and scientists would consistently refer to Celiac as a food allergy and Gluten as a food allergen.
When someone is buying food for Jax, preparing food for Jax, and/or serving food to Jax, we need to be able to clearly communicate to that person that Jax must avoid eating Gluten, since if he does eat just a crumb of Gluten, he will likely have an adverse health reaction. The simplest and most effective way to communicate this in Plain English is to say that Jax has a food allergy. Period. Full Stop! This is the way that people organically talk about food when it can cause an adverse health effect trough an immunological reaction.
Beyond Celiac has reported that 44% of people with Celiac Disease who follow a strict Gluten Free diet still get glutened once a month. According to the Celiac Disease Foundation ("CDF") and research published in the the American Journal of Gastroenterology, "the lifetime treatment burden of the Gluten Free diet is perceived by patients to be second only to end-stage renal disease, and by caregivers, comparable to caring for a patient with cancer." In April 2019, CDF's CEO Marilyn Geller's testified to Congress that "diagnosed patients report that they miss, on average, 23 days of work and school annually, resulting in excess utilization of our healthcare resources."
Unfortunately, in spite of our many precautions, Jax has been "glutened" at times through accidental ingestion of Gluten and that has resulted in him getting violently ill with severe GI adverse reactions commensurate with foodborne illness (food poisoning), and in addition, potential long-term complications including damage to his small intestine. In 2021, Jax got violently ill when the chef at a restaurant thought a packaged food product was Gluten Free since it did not have Wheat labeled on it, but the food product did have unlabeled Gluten in it. [2] [3] That’s one real world example of getting Glutened and why we need Gluten to be labeled on packaged foods! That's another reason why we need to stop gaslighting Celiac Disease as not a food allergy and Gluten as not a food allergen. That's why we need to label Gluten as a Major Food Allergen on all packaged foods in the U.S.
Capitol Hill Conversations - Celiac Confusion
Anecdotally, in conversations we have had with some Congressional staffers on Capitol Hill in 2022 about naming Gluten as the 10th Major Food Allergen, we received feedback that in looking at Gluten ingestion from a "biological perspective with some type of biological identifier," they said something to the effect "that the FDA does not consider Gluten as a food allergen since it does not cause anaphylaxis in people with Celiac."
As such, and in spite of the Food Allergen Labeling and Consumer Protection Act’s (FALCPA) Section 202 Findings about Celiac Disease, I also heard feedback that FALCPA was not the "right vehicle" to address our request for Gluten to be codified as the 10th Major Allergen and to be labeled on all packaged foods in the U.S.
The FALCPA does not define "allergy", "food allergy", "allergen", "allergic reaction" or "major allergen." FALCPA also does not mention "immunoglobulin E", "IgE", "IgE-Mediated", "Non-IgE-Mediated" "antibodies" or "anaphylaxis." Moreover, there is no express requirement in the FALCPA that a "Major Food Allergen" must include symptoms compatible with IgE-mediated mechanisms, including anaphylaxis.
It's no wonder that there is ingrained consumer and Congressional confusion. According to the FDA's Web site page entitled, "'Gluten-Free' Means What It Says," the FDA states that people with Celiac Disease "face potentially life-threatening illnesses if they eat gluten, typically found in breads, cakes, cereals, pastas, and many other foods… There is no cure for celiac disease and the only way to manage the disease is to avoid eating gluten." However, there is no mention that Celiac is a food allergy, digestive disease and/or auto-immune disease. There is also no mention that Gluten is a food allergen, and that Gluten causes an allergic reaction in people with Celiac Disease.
On April 19, 2022, the FDA published "Evaluating the Public Health Importance of Food Allergens Other Than the Major Food Allergens Listed in the Federal Food, Drug, and Cosmetic Act: Guidance for FDA Staff and Stakeholders – Draft Guidance", April 19, 2022, Docket number: FDA-2021-N-0553 ("FDA’s Draft Guidance").
Based on the collective response and findings from scientists, physicians, patient advocacy groups, as well those with Celiac Disease and their loved ones and caretakers, the number of public comments submitted to the FDA indicates a clarion call to declare Gluten as a Major Food Allergen and require that Gluten be labeled on all packaged foods. In total, there were 1,903 comments submitted to the FDA, and of those, 1,576 comments mentioned Celiac and/or Gluten as a food allergen (82.8%).
We appreciated the opportunity to share our lived experience and provide our organizations' comments from Bari Consulting Group, Celiac Journey and @GlutenFreeFinds_pa on the FDA’s Draft Guidance (“Bari Comments”). The Bari Comments are intentionally very detailed in order to aggregate a lot of seemingly disparate, yet related, historical, legislative, regulatory, legal, medical and moreover patient advocacy perspective information. The Bari Comments are designed to ensure that the record is very clear since the FDA's Draft Guidance suggests that time has a way of blurring perspective for the FDA when it comes to the Food Allergen Labeling and Consumer Protection Act of 2004.
With respect to the Celiac Disease community, which has been historically underserved and marginalized by our Federal government (i.e., underfunding medical research for Celiac Disease, labeling Gluten only with a voluntary scheme, disqualifying Celiacs from service in the military, excluding Celiac Disease from the CDC’s Index of Diseases & Conditions, etc.), the FDA’s Draft Guidance presented an inequitable evaluation framework, as well as perpetuated flawed scientific, governmental and societal biases including:
A Gluten Free diet is all that is needed to treat Celiac Disease, as opposed to all that has ever been historically available to treat Celiac Disease.
With respect to labeling food products in the United States, the voluntary Gluten Free labeling scheme sufficiently protects consumers who are on medically required and very restrictive Gluten Free diets, as opposed to all that has ever been historically utilized labeling-wise.
Othering the consumer protection needs for Celiacs in the United States with not evaluating the public health importance of Gluten as a food allergen because this Non-IgE-Mediated food allergy is not capable of triggering anaphylaxis and being immediately life-threatening, while seemingly ignoring that Celiacs face potentially life-threatening and severe adverse health effects that can arise through Gluten ingestion, including by way of example and not limitation: anemia, cancer, heart disease, immunological scarring, intestinal damage, malnutrition, etc.
FALCPA Has Failed Celiacs Based on a Big Lie - FALCPA Negotiations Were Scientifically Flawed From the Start with Celiac Being Incorrectly Othered as a Gluten Intolerance and Not as a Food Allergy:
On August 9, 2002, Inside Washington’s (Health Policy’s) FDA Week reported that Senator Kennedy floated an amendment to the FALCPA memorialized,
"But the food industry source says that even though the amendment goes in the right direction, the food industry continues to oppose the bill on the grounds that a mandatory approach is not appropriate or needed, and that instead the food industry should be allowed to continue to implement its voluntary guidelines... Critics of the bill [in the food industry] had charged that scientifically, Gluten is an intolerance not an allergen." (emphasis added)
On September 27, 2002, Inside Washington’s (Health Policy’s) FDA Week (page 5) memorialized,
"Substitute [bill] pulls mandatory Gluten declaration... This week the Senate Health Committee passed without objection a watered-down version of a bill that would require food processors to label the eight most common types of food allergens in plain English. The substitute version, unlike the underlying bill... would not require the declaration of Gluten." (emphasis added)
Notwithstanding the foregoing, no one from the FDA or HHS spoke up to protect Celiacs. This "science" was wrong in 2002, and it is wrong now in 2023. When FALCPA was signed into law in 2004, it had already left the Celiac community behind with a voluntary labeling scheme that would not be enacted until 2014, but moreover it was incongruent with the 1999 Codex Criteria and how the international community was already starting to require the labeling of Gluten on all packaged foods.
Dr. Virginia Stallings Joined the Clarion Call to Label Gluten Now
The Bari family was honored to have been joined at the FDA meeting by Dr. Virginia Stallings, a board-certified nutrition pediatrician, Professor of Pediatrics and Director of the Nutrition Center at the Children's Hospital of Philadelphia (where Jax is treated for Celiac) who along with the Baris has called for Gluten to be labeled as a Major Food Allergen. Dr. Stallings is very well known and respected by the FDA's senior leadership in the fields of nutrition, food allergies and labeling. Previously, Dr. Stallings served as the Editor and Chair of the National Academies of Sciences, Engineering, and Medicine, Committee on Food Allergies which published the 574 page seminal work that was funded by the FDA: "Finding a Path to Safety in Food Allergy: Assessment of the Global Burden, Causes, Prevention, Management and Public Policy."

With respect to labeling Gluten as a Major Food Allergen, Dr. Stallings opined,
"While a Non-IgE-Mediated food allergy does not trigger anaphylaxis and is not immediately life-threatening, people with Celiac Disease face potentially life-threatening and severe adverse health effects that can arise through gluten ingestion including by way of example and not limited to: anemia, cancer, heart disease, immunological scarring, intestinal damage and malnutrition… A gluten free diet is not all that is needed to treat Celiac Disease; rather a gluten free diet is all that has ever been historically available to treat Celiac Disease. Additionally, with respect to labeling food products in the United States, the voluntary gluten free labeling scheme does not sufficiently protect consumers who are on medically required and very restrictive gluten free diets. My strong recommendation is that gluten be labeled on all packaged foods in the United States, in accordance with the 2021 FAO/WHO Expert Consultation, just like it is in more than 85 countries around the world." (emphasis added)
The FDA's Bias Against Celiac
The FDA's Draft Guidance does not stand alone with its bias against Celiac. On the FDA’s "Food Allergen Labeling And Consumer Protection Act of 2004 Questions and Answers," dated December 12, 2005; Updated July 18, 2006 ("FDA's FALCPA FAQs"), the questions and answers suggest that Celiac Disease is an after-thought. The FDA's FALCPA FAQs also do not refer to Gluten as a food allergen, that Gluten causes an allergic reaction in people with Celiac Disease, or even mention the FALCPA’s Section 2, Findings ("FALCPA's Findings") that expressly discuss Celiac Disease as one of its six key findings. There are no other food allergens or diseases other than the Top 8 Major Food Allergens, Gluten and Celiac expressly mentioned in FALCPA’s Findings!
The FDA's FAQs suggest that Gluten is something other than a food allergen, "The following questions and answers will be useful in answering questions about FALCPA, food allergen labeling, gluten, and advice for consumers."
In FDA's FAQ 21 about FALCPA, the FDA seemingly goes out of its way to refer to a "concern" about Gluten (suggesting it is less serious than a food allergen) because Celiac is a "chronic digestive disease," Celiac is not a food allergy and Gluten is not a food allergen.
"Why is there a concern about gluten? Gluten describes a group of proteins found in certain grains (wheat, barley, and rye.) It is of concern because people with celiac disease cannot tolerate it. Celiac disease (also known as celiac sprue) is a chronic digestive disease that damages the small intestine and interferes with absorption of nutrients from food. Recent findings estimate that 2 million people in the U.S. have celiac disease or about 1 in 133 people." Note that the most current estimate from the NIH is that Celiac "affects greater than 1% of the US population [3.3+ million Americans], and incidence appears to have been increasing over the last several decades."
On the FDA’s "Gluten-Free Labeling of Foods" page, there is no mention that Celiac is a food allergy, digestive disease and/or auto-immune disease and that Gluten is a food allergen. There is also no mention that Gluten is a food allergen.
In the FDA’s "Temporary Policy Regarding Certain Food Labeling Requirements During the COVID-19 Public Health Emergency: Minor Formulation Changes and Vending Machines Guidance for Industry May 2020," the FDA once again othered Gluten as something else other than a food allergen,
"SAFETY: the ingredient being substituted for the labeled ingredient does not cause any adverse health effect (including food allergens, gluten, sulfites, or other ingredients known to cause sensitivities (see section C.2.a) in some people, for example, glutamates);" (emphasis added)
In the FDA's "Small Entity Compliance Guide: Gluten-Free Labeling of Foods," there is no mention that Celiac is a food allergy, digestive disease and/or auto-immune disease. There is also no mention that Gluten is a food allergen.
The National Institutes of Health also do not refer to Celiac Disease as a food allergy or Gluten as a food allergen. According to the NIH's NIDDK, "Celiac disease is a chronic digestive and immune disorder that damages the small intestine. The disease is triggered by eating foods containing gluten. The disease can cause long-lasting digestive problems and keep your body from getting all the nutrients it needs." (emphasis added)
According to the NIH’s NIAID, "Celiac disease is an autoimmune disease that occurs in genetically susceptible individuals who develop an immune response to ingested gluten." (emphasis added)
Even the Celiac Community Gaslights Celiac as Not a Food Allergy and Gluten as a Second Glass Allergen
"The difference between the right word and the almost right word is the difference between lightning and a lightning bug." -- Mark Twain
In addition to the FDA and NIH, there even appear to be various voices in the Celiac and IgE-Mediated food allergy communities who also seemingly go out of their way to say that Celiac is not a food allergy, a "true" food allergy or a "typical" food allergy. It's almost as if there is a pride of distinguishing Celiac as something unique in comparison to food allergies, even though we need the same consumer protections when it comes to labeling food products and avoiding cross-contamination.
According to Dr. Peter H.R. Green in "Celiac Disease (Newly Revised and Updated): A Hidden Epidemic," "Celiac disease is a delayed type of immune reaction – it is not a food allergy."
As a parent of a child with Celiac Disease and as a Columbia University alumnus, I have great respect for the work of Dr. Green, Director of the Celiac Disease Center at Columbia University. However, I respectfully disagree with Dr. Green and other thought leaders in the Celiac community and believe that they need to reimagine how they communicate about Celiac Disease.
Our extensive research has strongly suggested that not calling Celiac a food allergy and moreover not referring to Gluten as a food allergen has unintentionally hurt the Celiac community in myriad ways. Gaslighting Gluten as not being a food allergen and Celiac Disease as not being a food allergy because the immune response is a Non-IgE Mediated mechanism is just wrong, and stands in contrast to evidence-based science.
In terms of consumer protection, the Celiac community would benefit greatly if the FDA and scientists would consistently refer to Celiac as a food allergy and Gluten as a food allergen.
FARE (Food Allergy Research & Education) does not refer to Celiac as a food allergy and Gluten as a food allergen. FARE also does not discuss that Celiac can be life-threatening.
"Celiac disease is an autoimmune disease. Antibodies are produced in response to the presence of gluten resulting in inflammation and damage to the lining of the small intestine. Many symptoms involve the gastrointestinal tract (e.g., diarrhea, constipation, weight loss, abdominal pain and bloating). Other symptoms can include skin rashes and disorders that result from nutrient deficiencies. The estimated global prevalence of celiac disease is 1%, similar to wheat allergy."
While FARE has done amazing advocacy and education work to protect those with IgE-Mediated food allergies, FARE has not embarked on advocating for the labeling of Gluten as a Major Food Allergen. This appears to be because FARE's concentration follows the "orthodox" allergists who focus exclusively on IgE-Mediated food allergies that are potentially immediately life-threatening and can cause anaphylactic reactions, notwithstanding that a Gluten allergy with Celiac is potentially life-threatening (coupled with many other adverse health outcomes including intestinal damage), and the Celiac community needs the same consumer protections as the IgE-Mediated food allergy communities in terms of the required labeling of Gluten on all packaged foods.
As it pertains to the Celiac community, we need to reduce Gluten allergy stigma and disparities in consumer protection, along the lines of what the Department of Health and Human Services is working on with the HIV Challenge: Innovative Community Engagement Strategies to Reduce HIV-Related Stigma and Disparities.

History of Food Allergy Terminology
To understand the importance of naming, "[t]he word allergy has been around only since 1906, when Austrian pediatrician Clemens von Pirquet coined it to describe altered biological reactivity. It didn’t gain traction until the mid-1920s, when it took on a big-tent definition describing reactions to everything from food and insect stings to mold and hay fever, says medical historian Dr. Matthew Smith, author of the new book 'Another Person's Poison: A History of Food Allergy.' For most of the 20th century, research-focused orthodox allergists, who insisted on a definition requiring a measurable immune reaction, battled with more flexible food allergists, whose main focus was bringing relief to their patient’s hypersensitivities."
According to "Another Person's Poison: A History of Food Allergy" by Dr. Smith, the orthodox allergist movement was "represented by the AAAAI" and “worked with the food industry to reinforce their narrow definition of food allergy, a definition that was epitomized by peanut allergy. Forgotten in the focus on the acute, anaphylactic reaction to foods that food allergists had long argued were more common and problematic. Although some of these patients’ problems came to be understood in terms of intolerances to lactose or gluten, symptoms connected with food additives and refined foods continued to be viewed with suspicion in the face of mounting evidence that they could be harmful. Despite making food allergy a legitimate health concern, the rise of peanut allergy also helped to transform food allergy into a very specific, attenuated, and limited phenomenon, adhering to the way orthodox allergists had defined it all along."[4]
As Dr. Smith continued,
"Of course it was not just any food allergy the AAAAI had in mind; it was IgE-mediated, anaphylactic reactions to peanuts and a small number of other foods [footnote 13 – 'Some of these other foods will be discussed later in this chapter, but included in their number were milk, egg, wheat, seafood, soya, nuts, and wheat. [sic]']… Much as orthodox allergists had heralded the emergence of IgE for giving allergy legitimacy, peanuts made food allergy respectable, thrusting it into the spotlight like never before. Peanut allergy made that matter."
This is a great example which shows how the American Academy of Allergy, Asthma & Immunology has othered the consumer protection needs of the Celiac community by gaslighting Celiac Disease and saying that there is no such thing as a Gluten allergy. In other words, the "orthodox allergists" worked to define food allergy in the US as limited to IgE-Mediated reactions that can cause anaphylaxis, and in turn excluded Celiac Disease, which is a Non-IgE-Mediated food allergy, from the same consumer protections as IgE-Mediated food allergies.
"Gluten is a protein found in grains, such as wheat, barley and rye. Some people are allergic to wheat, but that is not the same as a gluten allergy. Gluten allergy is a misleading term commonly confused with wheat allergy, or sometimes celiac disease. There is no such thing as a gluten allergy, but there is a condition called Celiac Disease." (emphasis added)

It's important to understand that when Celiac is othered and not referred to as a food allergy and when Gluten is not referred to as a food allergen, then those who have Celiac and their caretakers are effectively excluded from the following ecological-developmental model for food allergies as detailed in the diagram. Such exclusion negatively impacts quality of life, equity in participation in one of life’s daily activities -- eating, consumer protections with labeling, medical research, etc.
Legislative History of Federal Food Drug and Cosmetic Act of 1938: Allergy Is "One of Those $14 Words That Physicians Coin"
The legislative history of the FDCA [Federal Food Drug and Cosmetic Act of 1938] sheds light on the newness of the concept of "food allergy" in 1934. In some ways, what's old seems new again when it comes to naming conventions, consumer behavior and consumer protection for food allergies. The following dialogue occurred between the Commissioner of FDA Mr. Walter Campbell, U.S. Senator Felix Hebert who served from 1929-1935 (R, RI), and Senator Royal Samuel Copeland, MD who served from 1923-1938 (D, NY) during a Congressional hearing in 1934 regarding proposed new food and drug legislation: [5]
“Mr. Walter Campbell [FDA Chief]: I do not think you heard, and I am sorry that you and the entire committee did not hear Dr. Brown, of Washington, an expert on hypersensitivity, testify yesterday afternoon. He pointed out this, that he had a child in his office who was suffering from allergy. I don’t know whether the cause was eggs or milk.
Senator Hebert: What was that word, allergy?
Mr. Campbell: Yes; allergy.
Senator Hebert: How do you spell it?
Mr. Campbell: A-l-l-e-r-g-y.
Senator Hebert: What is the definition of it? I heard the term a number of times and I admit my ignorance. Now, I ask you to explain it to me.
Mr. Campbell: You need not feel humiliated, because it is not in the dictionary, or at least it is not in those that I have consulted. It is a medical term. It means the hypersensitivity of certain individuals to certain protein products. It may manifest itself in the form of asthma or hives or other forms of physical distress.
Senator Copeland: What is food for one is poison for another.
Mr. Campbell: That is right.
Senator Hebert: I would like to look up the derivation of that word. Senator Copeland: Here is a book on the subject. Senator Hebert: All right. I suppose it is one of those $14 words that physicians coin.”[6]
(emphasis added)
The term "food allergy" is generally understood as a term for any form of negative or adverse reaction. The use of the term "food allergy" has become a generic term by the public to describe any form of adverse reaction from food. This is just like when someone uses the word Kleenex to ask for a tissue, they are just using the word Kleenex in a generic manner, even though Kleenex is a registered trademark for a brand of tissue. Consumers (lay people) do not parse food allergen and food allergy terminology into IgE-Mediated and Non-IgE-Mediated mechanisms when it comes to understanding food labels and other consumer protections needed.
Let's fast forward from FDA Commissioner Campbell's Senate testimony in 1934 with the use of Plain English to describe allergy as a "medical term" that "means the hypersensitivity of certain individuals to certain protein products" to FDA Commissioner Califf's opening plenary remarks at the White House Conference on Hunger, Nutrition, and Health Regional Listening Session. Commissioner Califf spoke about getting information across to over 300 million people with all different reading levels, different languages, different ages, etc., including for the health of children like my son Jax who cannot eat Gluten and needs Gluten labeled on all packaged foods to keep him safe.
“A key revelation for me last time through as FDA Commissioner, this is my second stint, but last time through was the idea of getting information across to over 300 million people with all different reading levels, different languages, different age, really a difficult issue that we are working on very hard at the FDA, but we need to all work on it as a community. This is especially important when it comes to the health of children. For instance, we are focused on supporting the availability of foods that provide important nutrients essential for growth and development and reducing our exposure of young children to toxic elements like lead, arsenic, mercury, and cadmium in the foods they eat which can be harmful to their neurological development."[7]
It is also instructive to understand the semantic context of allergy, food allergen and allergic reaction with regard to the way a reasonable person conversant with relevant social and linguistic practices have used the words and what those words mean in society.
When we use the term food allergy, we intend it to mean an immunological reaction (i.e., Celiac Disease) to normally tolerated food proteins defined as food allergens (i.e., Gluten). By way of example, when we eat out at a restaurant with my son, we inform the server that he has a "severe allergy to Gluten" since the average reasonable person understands that he cannot eat Gluten. As previously discussed, the simplest and most effective way to communicate this in Plain English is to say that Jax has a Food Allergy. Period. Full Stop.
If we had to explain in detail that he cannot eat Gluten because he has an autoimmune disease that attacks his small intestine when he eats Gluten, most people would say that he is allergic. However, it feels like every time we refer to it as a Gluten allergy, there is a societal bias that flows from the FDA and Federal government's bias that Celiac is not a food allergy, an allergic reaction to Gluten is much less serious than a typical IgE-Mediated food allergy, and that Gluten is not a food allergen.
Mechanism in Action – Cognitive Mechanism
As discussed herein, in medicine, mechanism in action is used to describe how for example a drug or food allergen in this case produces an effect in the body. When it comes to consumer protection and requiring that Gluten be labeled for those with a Celiac food allergy to Gluten, the FDA’s Draft Guidance seems incorrectly fixated on whether or not a food allergy is an IgE-Mediated Mechanism or Non-IgE-Mediated Mechanism.
I would suggest that the FDA also view this evaluation of the public health importance of food allergens other than the Major Food Allergens through a more equitable lens and focus also on cognitive mechanisms. With respect to selecting safe foods to consume, including reading food labels, cognitive mechanisms involve the ways in which people receive information, and the ways in which people think about, interpret, evaluate and therefore act upon that information received on food labels ("Cognitive Mechanism"). In marketing, we refer to that as part of consumer behavior.
Before there can be an IgE-Mediated or Non-IgE-Mediated mechanism, there is a Cognitive Mechanism that takes place with selecting safe foods to consume and reading labels. What happens inside the body is a secondary mechanism in action, and as such, cannot be exclusively viewed through that downstream mechanism lens without regard to the initial and primary Cognitive Mechanism, followed by an Ingestion Mechanism.
According to the research entitled, "The Food Allergy Consumer Journey, Defining Challenges, Overcoming Obstacles, Creating a Blueprint for Food Allergen Labeling Success" conducted by McKinsey & Company, Northwestern University and Global Strategy Group for Food Allergy Research & Education (FARE), 71% of consumers "check food labels every time they shop – some for 3-5 minutes per product." We can personally attest to that time commitment per product that we spend in trying to purchase safe food products for our 9 year old son, especially in the absence of mandatory labeling of Gluten.
Labeling Food Allergies
When it comes to labeling (naming, categorizing) food allergies, I agree in principle with Mun Cho, registered dietitian, that the way we currently talk about food allergies minimizes the visibility of Non-IgE-Mediated food allergies, and the impact they have on families. For example, Cho wrote,
"Strict avoidance of the food trigger is a must, regardless of the type of food allergy. Parents must be vigilant with label reading and avoiding cross contact. The social, emotional and financial burden of food allergies are real, and they do not discriminate between the two types [IgE-Mediated and Non-IgE-Mediated]." (emphasis in original)
"So why does the language we use matter? It shapes the way we perceive and communicate. The way we currently talk about food allergies minimizes the visibility of non-IgE food allergies, and the impact they have on families. To the healthcare providers reading this, please do not take what I’m saying as a criticism. My hope is that we can change the way we talk about food allergies so that we do so in a more inclusive manner."
Labeling Gluten as Something Else Other than a Food Allergen Has Had Consequences in Terms of Undermining Perceptions of the Public Health Importance of Consumer Protections for Celiacs
The Boston Globe reported on how some servers in restaurants do not take the Gluten food allergy seriously and put people's lives at risk because they did not perceive Celiac as a true food allergy, but instead as a joke; they perceived a Gluten Free diet request as a preference and not a medical requirement. It is my contention that the FDA and the Federal government's historical underserving of the Celiac community has helped perpetuate these governmental and societal biases by not using proper and consistent terminology to indicate the seriousness and life-threatening nature of Celiac Disease and the need for Gluten to be declared as a Major Food Allergen, let alone a food allergen.
"Recall what a former cook at the Tavern on the Green in New York’s Central Park copped to a few years back. Alleging that customers’ gluten problems were all in their 'disturbed little heads,' Damian Cardone boasted he had made a habit of secretly giving anyone ordering gluten free pasta the normal stuff with gluten and that they were no worse for it. (He seemed clueless that the most serious damage that celiac patients suffer takes place over time, not immediately.)
Then there was the waitress who posted an anonymous screed on Reddit that went viral. It began: A server will never say this to your face but we all know your gluten allergy is fake…. You are just on a gluten-free diet and want attention. When I track down the author, Chelsea Welch, she admits she had written the post in frustration, after witnessing too much nonsense as a waitress in an Italian restaurant in St. Louis."
Foodborne Illness Provides an Analogy for Umbrella Terminology for “Food Allergy” and “Food Allergen”
The FDA and the Federal government must view food allergy in a collective sense that does not exclude or other Gluten as a less serious food allergen compared to the Major Food Allergens. The FDA and the Federal government must also expressly communicate the terms "food allergy" and "food allergies" in a collective sense that does not exclude or other Celiac as a less serious food allergy or Gluten as a less serious food allergen.
Let's look at the terminology involving foodborne illness in the context of consumer protections. There are many different disease-causing germs that can contaminate foods, so there are many different foodborne infections (also called foodborne disease or food poisoning). The key to understand here is that these are all referred to as foodborne illness, foodborne disease or food poisoning. The use of different terminology is not about creating a hierarchical level of importance or othering some forms of foodborne illness as less severe and therefore meritorious of less consumer protections.
According to the CDC, "anyone can get food poisoning, but certain groups of people are more likely to get sick and to have a more serious illness. Their bodies' ability to fight germs and sickness is not as effective for a variety of reasons. These groups of people are: Adults Aged 65 and Older, Children Younger Than 5 Years, People with Weakened Immune Systems, and Pregnant Women." Further, we do not other foodborne illness protections because some people may be more likely to get foodborne illness. To the contrary, we strive to protect everyone against foodborne illness, but call out the special and incremental needs of those at-risk communities.
Type 1 Diabetes Was Once Called Juvenile Diabetes
In December 2024, the Clinical Gastroenterology and Hepatology journal from the American Gastroenterological Association published in-depth research finding that there is a high risk of digestive cancers in patients with Celiac Disease, and there is also a significant increased risk for other adverse health issues including Type 1 Diabetes.
From a naming perspective, it is instructive to understand that Type 1 Diabetes was formerly known for many years as Juvenile Diabetes. This evolved over time from Juvenile Diabetes to T1D since in part diabetes can impact people of all ages.
People's Words & Actions Can Shape Your Brain
In her thought-provoking TED talk, Lisa Feldman Barrett, PhD, Professor of Psychology at Northeastern University, shared some of revolutionary research in psychology and neuroscience.
"Why do the words you encounter have such wide-ranging effects inside you? Because many brain regions that process language also control the insides of your body, including major organs and systems that manage your body budget.
These brain regions are contained in what scientists call the 'language network' and guide your heart rate up and down. They adjust the glucose entering your bloodstream to fuel your cells. They change the flow of chemicals that support your immune system.
The power of words is not a metaphor; it’s in our brain wiring. We see similar wiring in other animals; for example, neurons that are important for birdsong also control the organs of a bird's body.
Words, then, are tools for regulating human bodies. Other people's words have a direct effect on your brain activity and your bodily systems, and your words have that same effect on other people. Whether you intend that effect is irrelevant. It's how we’re wired.
Does this mean that words can be harmful to your health? In small doses, not really. When someone says things you don't like, insults you or even threatens your physical safety, you might feel awful.
Your body budget is taxed in that moment, but there's no physical damage to your brain or body. Your heart might race, your blood pressure might change, you might ooze sweat, but then your body recovers and your brain might be a bit stronger afterward.
Evolution gifted you with a nervous system that can cope with temporary metabolic changes and even benefit from them. Occasional stress can be like exercise — brief withdrawals from your body budget followed by deposits create a stronger, better you.
But if you are stressed over and over and over again without much opportunity to recover, the effects can be far more grave. If you constantly struggle in a simmering sea of stress and your body budget accrues an ever-deepening deficit, that’s called chronic stress. It does more than just make you miserable in the moment.
Over time, anything that contributes to chronic stress can gradually eat away at your brain and cause illness in your body."
Words matter when it comes to Celiacs being able to communicate with others that they have a food allergy to Gluten and when it comes to Celiacs relying on food labels to keep them safe. Let's label Gluten as a Major Food Allergen in the US, just like it is done in 85 countries worldwide.
Notes
[1] This diagram graphic is intended to convey that Non-IgE-Mediated food allergy with Celiac Disease and typical IgE-Mediated food allergies are both really dangerous and deserve equal treatment with respect to consumer protection with food labeling. The adverse health effects are listed in alphabetical order, and these health dangers are an illustrative, but not exhaustive list. This diagram expands and updates information as was included in Table 2-1 in the National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee on Food Allergies. “Finding a Path to Safety in Food Allergy: Assessment of the Global Burden, Causes, Prevention, Management and Public Policy, Committee on Food Allergies: Global Burden, Causes, Treatment, Prevention, and Public Policy, Food and Nutrition Board, Health and Medicine Division, Virginia A. Stallings and Maria P. Oria, Editors” November 2016.
[2] See “Food Allergen Labeling And Consumer Protection Act of 2004 Questions and Answers”, Question 26, “What about food prepared in restaurants? How will I know that the food I ordered does not contain an ingredient to which I am allergic? FALCPA only applies to packaged FDA-regulated foods. However, FDA advises consumers who are allergic to particular foods to ask questions about ingredients and preparation when eating at restaurants or any place outside the consumer’s home.” [3] The CDC has estimated that fewer than half of the members of the restaurant staffs surveyed in 278 restaurants had received training on food allergies. Taking that into account, it is suggested that even less understand about Celiac as a food allergy and Gluten as a food allergen, in part since Celiac often gets conflated with a voluntary Gluten Free diet.
[4] Smith, Matthew. “Another Person's Poison: A History of Food Allergy.” New York: Columbia University Press, 2015. Print, pages 155-156.
[5] Derr, Laura E. “When Food Is Poison: The History, Consequences, and Limitations of the Food Allergen Labeling and Consumer Protection Act of 2004.” Food and Drug Law Journal, vol. 61, no. 1, 2006, pp. 65–165, http://www.jstor.org/stable/26660870. Accessed 16 May 2022.
[6] "Hearing Before the Senate Comm. on Commerce, 73d Cong. (1934) (statement of Walter G Campbell, Chief of FDA), reprinted in Dunn, supra note 170 [Hearing Before the S. Comm. on Commerce, 73d Cong. (1934) (statement of Walter G. Campbell, Chief of FDA), reprinted in Charles Wesley Dunn, Federal Food, Drug, and Cosmetic Act: A Statement of Its Legislative Record 1176 (1987).], at 1176."
[7] Robert Califf, M.D., Commissioner of the FDA stated in opening plenary remarks at the White House Conference on Hunger, Nutrition, and Health Regional Listening Session, June 7, 2022.



